Granzow Suction Assisted Protein LipectomySM (Granzow SAPLSM) for Advanced Lymphedema of the Arm or Leg
Granzow Suction Assisted Protein LipectomySM (Granzow SAPLSM) surgery is part of Dr. Granzow’s comprehensive Granzow SystemSM lymphedema program. Since 2010, Dr. Granzow has been performing his unique Granzow SAPLSM surgeries to achieve safe and dramatic reductions of the affected arms or legs in hundreds of patients with advanced, stage 2 lymphedema.
Granzow SAPLSM lymphedema surgery performed by Dr. Granzow achieves a consistent average overall reduction of excess volume of approximately 86% in legs and 111% in arms and effectively normalize the size of the affected arm or leg in most patients. Dr. Granzow has published these impressive results in prestigious medical journals. Such consistent volume reductions are far superior to those possible with other surgery or treatment methods such as VLNT or LVA in patients with stage 2 lymphedema. Patients experience permanent volume reductions with Granzow SAPLSM surgery as part of the Granzow SystemSM treatment program.
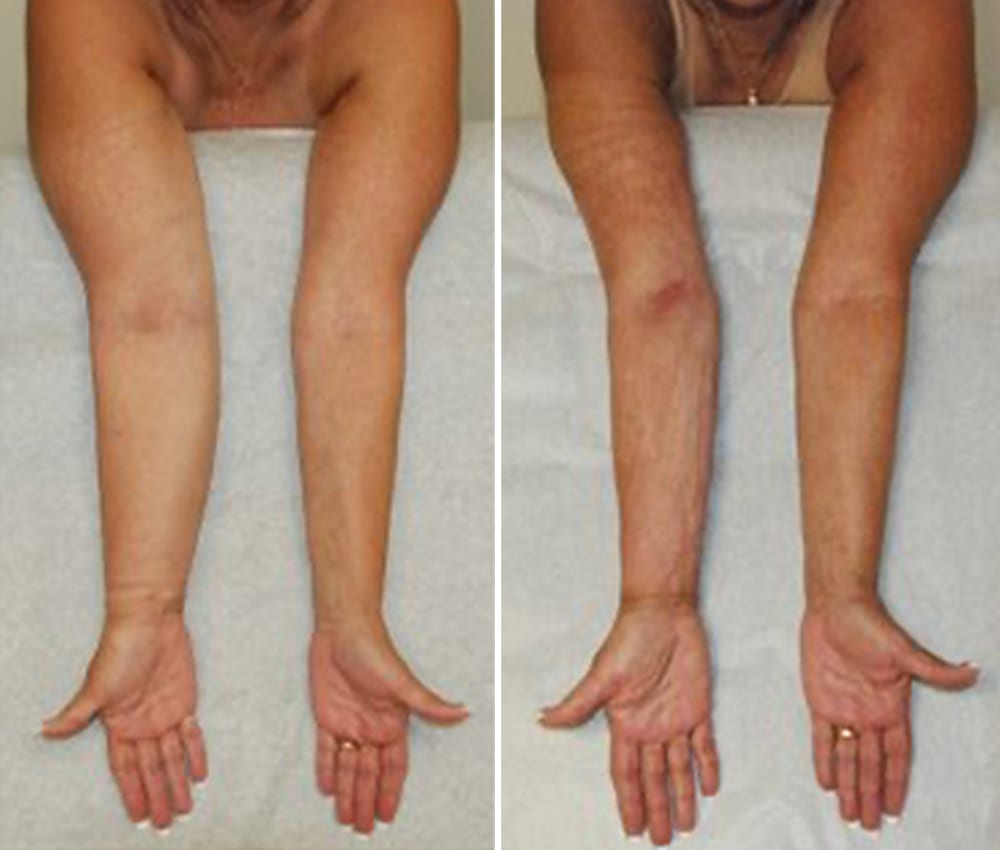
Patient with a prior 17-year history of non-pitting lymphedema of the right arm, treated with Granzow SAPLSM. After treatment, the affected right arm is now slightly smaller than the unaffected left side.
Innovative Granzow 2-PhaseSM Method to Reduce Both Lymphedema Volume and Symptoms
Dr. Granzow has pioneered the Granzow 2-phaseSM combination of Granzow SAPLSM surgery with VLNT and LVA surgeries to achieve both volume reduction and also significant reductions in compression garment use and lymphedema therapy. He was the first surgeon to successfully perform Granzow SAPLSM with subsequent VLNT and LVA surgeries for the same patient to normalize the size of the arm or leg and also reduce the requirement for postoperative garment use and lymphedema therapy.
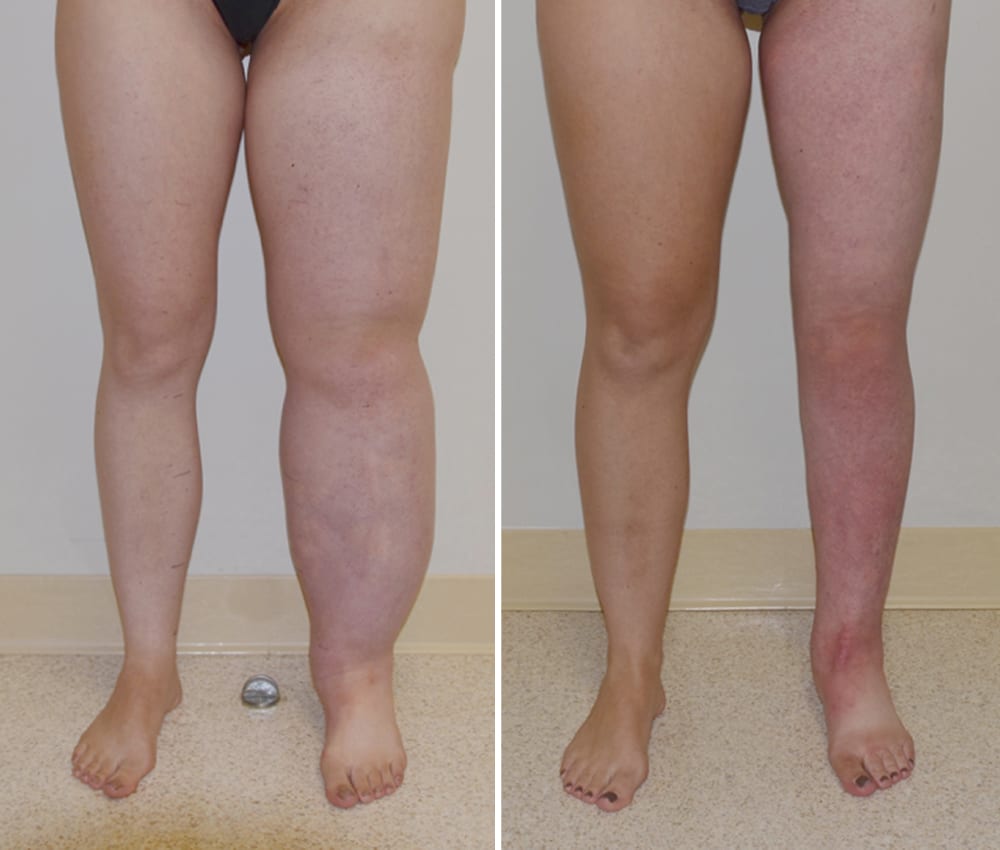
Patient 18 Months After Lymphatic Liposuction and 7 Months After Vascularized Lymph Node Transfer.
A volume reduction of over 80% was achieved and a compression garment is no longer worn during the day. This reduction has been maintained for over 10 years after surgery.
Why Granzow SAPLSM Surgery for Stage 2 Lymphedema Patients?
VLNT and LVA surgeries by themselves cannot significantly reduce the solid volume excess found in late, stage 2, lymphedema. Dr. Granzow performs his unique Granzow SAPLSM lymphedema surgery to remove these solids permanently. In these patients, the lymphedema disease process has progressed to such an extent that the lymphatic system has broken down and permanent solids have accumulated. In many cases, the affected arm or leg may feel soft, and careful examination by a trained expert may be required to differentiate soft solid from soft fluid in the affected area.
Granzow SAPLSM is NOT Cosmetic Liposuction
It is critical to note that Granzow SAPLSM is different from cosmetic liposuction techniques. The indications, equipment, therapy integration before, during and after surgery and surgeon training and experience are all unique. A team-based approach with an experienced surgeon and trained lymphedema therapist is required. Cosmetic or similar liposuction used to treat lymphedema or used as an “adjunct” technique will be expected to produce poor results.
Granzow SAPLSM is Safe

Example of material removed during Granzow SAPLSM surgery. The volume and character of the pathologic fluids which accumulate in stage 2 lymphedema are different than regular fat removed with cosmetic liposuction.
Dr. Granzow’s Granzow SAPLSM lymphedema surgery has been proven to produce safe and consistent results and the research results are published in prominent medical journals. The lymphatics in the arm or leg are not damaged by the surgery. In fact, the reduction of excess fats and pathologic solids decreases inflammation and improves the lymphatic drainage of the limb and considerably improves the management of the affected areas.
Peer-reviewed papers in the medical literature have shown that Granzow SAPLSM has been shown to significantly decrease the incidence of infections and cellulitis after surgery. Studies specifically looking at the lymphatic system before and after Granzow SAPLSM also have shown that Granzow SAPLSM does not damage lymphatics in an arm or leg affected by lymphedema.
In our experience with our Granzow SAPLSM surgical technique is that the need for compression garment use in Graznow SAPLSM patients did not increase after Granzow SAPLSM surgery. In fact, we have found that the inflammation in the soft tissues and lymphatic system greatly improves after Granzow SAPLSM surgery. Also, as mentioned above, Dr. Granzow can perform other techniques such as VLNT and LVA once healing after Granzow SAPLSM surgery is complete to further reduce the need for compression garment use.
Granzow SAPLSM and Obesity
Massive obesity on its own has been shown to cause lymphedema, and multiple theories exist to explain the decreased lymphatic function in severely overweight arms and legs. Significantly overweight patients are not appropriate surgical candidates for lymphedema surgery. However, weight loss itself has been shown to improve such lymphedema.
If you would like more information about Granzow SAPLSM surgery, please contact our Center of Excellence to schedule a consultation.