Overview of Lymphedema
Lymphedema is a disorder of the lymphatic system, which is an important part of the immune system. While Lymphedema can occur spontaneously (congenital, or primary lymphedema), most cases of lymphedema in the United States result from treatment for cancer with surgery, radiation, or both (secondary lymphedema).
In an arm or leg, the lymphedema commonly can cause:
- Devastating, rapidly spreading infections
- Severe swelling
- Loss of mobility and function
- Pain and discomfort
- Emotional distress
- Interference with work and daily activities
Progression of Lymphedema
The lymphatic system involves a circulation of lymphatic fluid, called lymph. Lymphedema occurs when the circulation and drainage of lymph is disrupted, such as after surgery or radiation therapy. Initially, the damage to the lymphatic system can be seen only with specialized imaging methods such as lymphoscintigraphy or indocyanine green (ICG) mapping, and is called stage 0 lymphedema.
As the lymphedema progresses, the lymph accumulates and causes swelling. This swelling can be treated with conservative therapy, and the affected arm or leg intermittently may reduce in size to a normal size. Surgeries that reduce lymph buildup, include vascularized lymph node transfer (VLNT) or lymphaticovenous anastomoses (LVA), can be effective at this stage if performed by an experienced lymphedema surgeon. This is called stage 1 lymphedema.
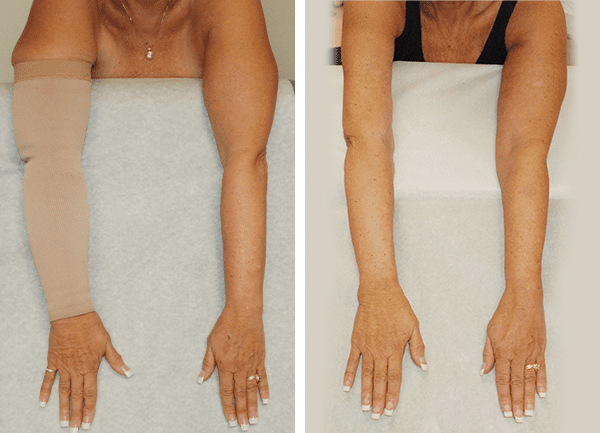
Reductions in size and compression garment use continue to be permanent almost 10 years after Granzow SystemSM surgery.
The lymph is very toxic and causes tremendous inflammation and damage to the surrounding tissues if it is not cleared. This makes infections, also called cellulitis, more likely and more dangerous. This inflammation results in deposits of additional solids and fat in the affected area. The affected arm or leg no longer reduces to a normal size. Such solid deposits are permanent and therefore the swelling they cause can no longer be reduced by conservative measures that move fluid, such as compression, manual lymphatic drainage, or surgeries such as VLNT or LVA that are designated to drain fluid. The solids can only be removed by surgery such as Granzow Suction Assisted Protein LipectomySM (Granzow SAPLSM). This is known as stage 2 lymphedema.
Secondary Lymphedema (more common)
Secondary lymphedema occurs from an external cause, such as surgery or radiation to treat cancer, or trauma. Infections from parasites can also cause secondary lymphedema, but this is extremely rare in the United States and other developed countries. In the cases of arm swelling, lymphedema usually tends to occur after treatment for breast cancer. It’s estimated that between 5% to over 50% of patients who have treatment for breast cancer that involves surgery to remove the lymph nodes as well as radiation therapy develop lymphedema in the arm to some degree.
Secondary lymphedema can also occur in the leg. This is most commonly due to treatment for gynecological cancer, such as cervical, uterine, or ovarian cancer. This includes cancer treatment with radiation and/or surgery to remove lymph nodes. It is estimated that approximately 20% of patients that have surgery to remove lymph nodes and have radiation therapy will develop some form of leg lymphedema. Male patients can also have lymphedema after cancer treatments, especially radiation therapy and lymph node dissection surgeries.
Primary Lymphedema (less common)
Lymphedema Worldwide
Worldwide, filariasis, a parasitic infection transmitted mainly by mosquitos, is the most common of lymphedema. This is important especially in countries such as India. Such parasitic infections are very rare in developed countries such as the USA where they mostly occur in individuals returning from travel to affected areas.
In developed countries, primary lymphedema accounts for around 10%-15% of lymphedema cases, while secondary lymphedema accounts for the remainder. The most common causes of secondary lymphedema in developed countries, such as the United States, are lymphadenectomy (lymph node dissection), radiation, infection, compression, trauma, burns, vascular surgery or tumor invasion.
The Obesity Revolution Podcast
To see the results of the procedure view or before and after gallery or schedule a consultation at our Center of Excellence today to learn more about Lymphedema.
